General information
Causes of knee joint disease
- Injuried. Approximately 20-30% of cases of knee arthropathy are related to a previous injury: tibial fractures (especially intra-articular fractures), meniscal injuries, torn or ruptured ligaments. Typically, knee arthrosis occurs 3-5 years after a traumatic injury, but it is also possible to present earlier disease - 2-3 months after the injury.
- Physical exercise. The manifestations of knee joint disease are usually related to excessive load on the joints. After the age of 40, many people understand that to maintain good physical condition, regular physical exercise is required. When starting to exercise, they do not take into account age-related changes and place unnecessary load on the joints, leading to the rapid development of degenerative changes and the appearance of symptoms of knee arthrosis. Running and strenuous, rapid squats are especially dangerous to the knees.
- excess weight. With excess weight, joint load increases, making microtrauma and major injuries (meniscal tears or ligament tears) more likely to occur. Arthropathy is particularly difficult in obese patients with severe varicose veins.
onset
Classification
- The first stage– The first manifestations of knee arthropathy. It is characterized by periodic dull pain that usually occurs after a large load is placed on the joint. There may be slight swelling in the joint, but this will go away on its own. No deformation.
- second stage– Increased symptoms of knee joint disease. The pain becomes longer and more severe. A crunching sound is often heard. There is slight or moderate limitation of movement and slight deformation of joints.
- The third phase– Clinical manifestations of knee arthropathy reach their maximum. The pain is almost constant and gait is impaired. The ability to move is significantly limited and the joints are deformed significantly.
Symptoms of knee joint disease
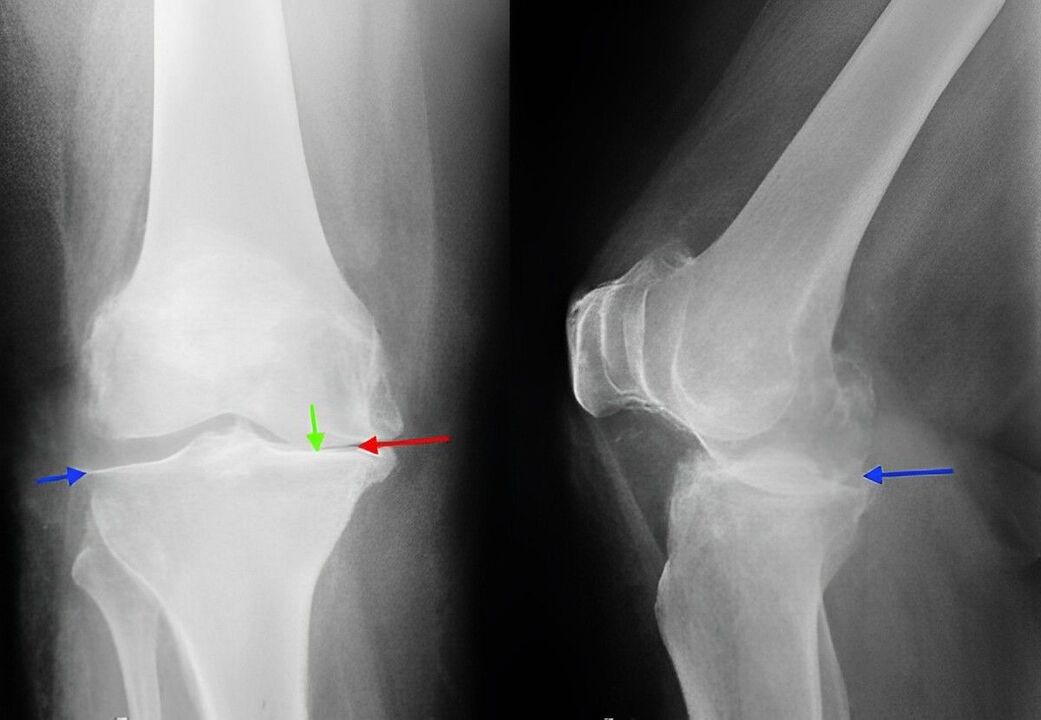
diagnosis